Blood-clotting condition cerebral venous thrombosis (CVT), which can cause irreversible brain damage, is significantly associated with mRNA Covid jabs, an official study in leading medical journal Vaccines has concluded.
Scientists analysed 1,154,023 adverse event reports from more than 130 countries logged with VigiBase, the World Health Organisation’s global database, and discovered a “potential safety signal for CVT occurrence after COVID-19 mRNA vaccination”.
The researchers warn that many reports were in younger people and the conditions were serious: “CVTs were commonly reported in patients aged 18-44 and 45-64 years, more frequently in women, and mainly in Europe and America… More than 90% of the patients were in serious condition, and 33% did not recover or died.”
Infowars.com reports: The researchers take into account under-reporting to produce estimates of increased risk above a baseline: around 3.5 times greater risk for mRNA vaccines and seven times greater risk for AstraZeneca. This means the CVT risk from mRNA vaccines, while high, is around half that of AstraZeneca.
They also found that CVT following mRNA vaccination is only around a third as deadly as that following AstraZeneca vaccination. This means mRNA vaccines lead to deadly CVT around a sixth as often as AstraZeneca, which may explain why the condition is particularly associated with the AstraZeneca jab.
The researchers cite earlier studies to suggest the mechanism relates to the spike protein binding to the wall of blood vessels, particularly in the brain, and activating clotting mechanisms.
There are few reports on CVT after mRNA-based COVID-19 vaccination. These studies suggested that CVT occurrences related to mRNA-based COVID-19 vaccines may be due to endothelial dysfunction caused by spike glycoprotein interactions with endothelial cells resulting in immunothrombosis. If the spike glycoprotein of mRNA-based COVID-19 vaccines binds to the angiotensin-converting enzyme 2 receptor, several inflammatory and thrombogenic molecules, such as leukocyte chemotactic factors, cell adhesion molecules (vascular cell adhesion molecule 1 and intercellular adhesion molecule 1), and procoagulant cytokines, can be activated. This mechanism may cause endothelial dysfunction, particularly in brain endothelial cells, which could contribute to a significant disruption of brain endothelial barrier integrity, ultimately promoting thrombus formation. Moreover, a previous study suggested that the spike glycoprotein may induce platelet aggregation and activation and eventually result in thrombus formation. Although the period of time in which the spike glycoprotein persists has not been clearly established, several studies have suggested that it may last for weeks. Thus, spike glycoprotein-related platelet activation triggered by mRNA-based COVID-19 vaccines could explain the trend of CVT occurrences after mRNA-based COVID-19 vaccinations. Furthermore, in line with these previous case reports, our results showed that CVT occurred mainly within a few weeks of mRNA-based COVID-19 vaccinations.
Here is the study abstract, summarising the findings.
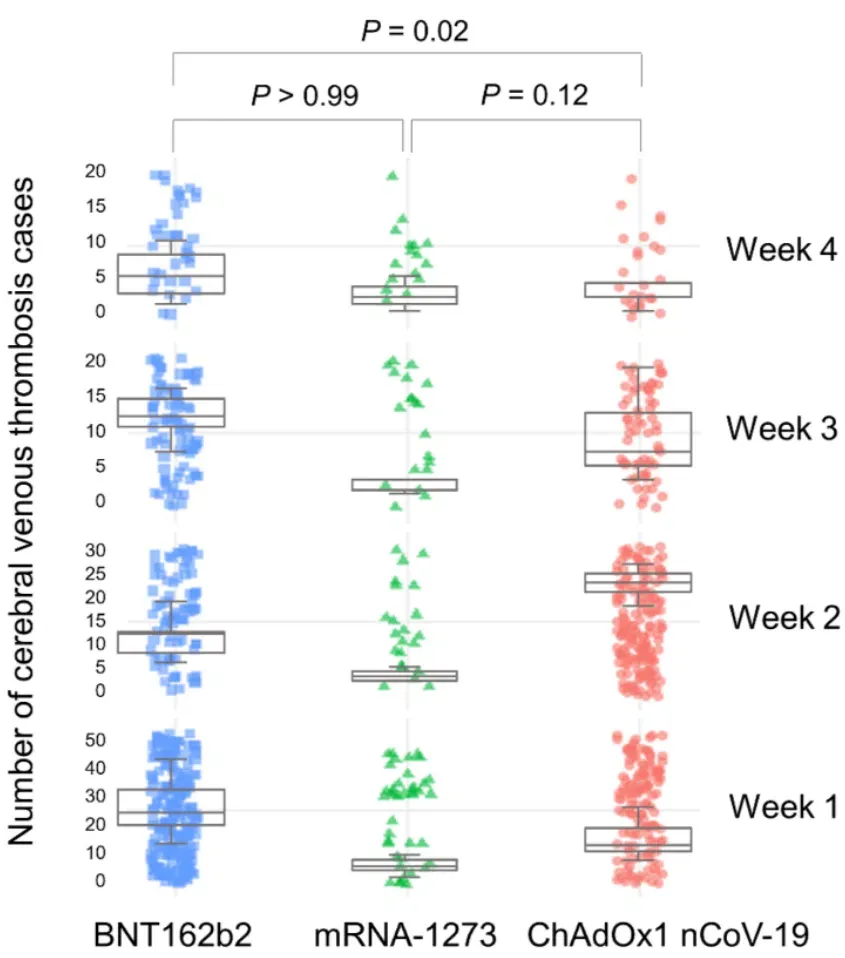
Cerebral venous thrombosis (CVT), a rare thrombotic event that can cause serious neurologic deficits, has been reported after some ChAdOx1 [AstraZeneca] nCoV-19 vaccinations against coronavirus disease 2019 (COVID-19). However, there are few reports of associations between COVID-19 mRNA vaccination and CVT. We retrospectively analysed CVT occurrence, time of onset after vaccination, outcomes (recovered/not recovered), and death after COVID-19 vaccination from adverse drug reactions (ADR) reports in VigiBase. A disproportionality analysis was performed regarding COVID-19 mRNA vaccines (BNT162b2 [Pfizer] and mRNA-1273 [Moderna]) and the ChAdOx1 nCoV-19 vaccine. We identified 756 (0.07%) CVT cases (620 (0.05%) after BNT162b2 and 136 (0.01%) after mRNA-1273) of 1,154,023 mRNA vaccine-related ADRs. Significant positive safety signals were noted for COVID-19 mRNA vaccines (95% lower end of information component = 1.56; reporting odds ratio with 95% confidence interval (CI) = 3.27). The median days to CVT onset differed significantly between the BNT162b2 and ChAdOx1 nCoV-19 vaccines (12 (interquartile range, 3-22) and 11 (interquartile range, 7-16), respectively; p = 0.02). Fewer CVT patients died after receiving mRNA vaccines than after receiving the ChAdOx1 nCoV-19 vaccine (odds ratio, 0.32; 95% CI, 0.22–0.45; p < 0.001). We noted a potential safety signal for CVT occurrence after COVID-19 mRNA vaccination. Therefore, awareness about the risk of CVT, even after COVID-19 mRNA vaccination, is necessary.
The association of blood-clotting adverse reactions with adenovirus vector vaccines like AstraZeneca and Johnson and Johnson have led to them being restricted or withdrawn in many countries, most recently by the U.S. FDA. The fact that this adverse reaction is also associated with mRNA vaccines, albeit in a somewhat less deadly form, suggests that the differential treatment of the two vaccine types on this basis is unlikely to be tenable.